Diagnostic Services British Columbia / Yukon Year In Review 2021
Senior Staff and Contact Information
|
Laboratory Medical Director Gwen Clarke, MD, FRCPC |
Laboratory Medical Director Matthew Yan, MD, FRCPC |
|
Diagnostic Services Manager Lhevinne Ciurcovich, MLT |
Assistant Manager, Diagnostic Services Heba Abukhadra, MLT |
|
Supervisor Vivian Stephens, MLT |
Diagnostic Services Laboratory Phone# 604-707-3434 |
|
Diagnostic Services Website |
Figures
- Figure 1: Total Number of Perinatal Specimens Tested between 2017 and 2021
- Figure 2: Total Number of Clinically Significant Perinatal Antibodies Detected between 2017 and 2021
- Figure 3: Frequency of Clinically Significant Antibodies Detected between 2017 and 2021
- Figure 4: Total Reference Specimens Tested by Edmonton Reference Laboratory between 2017 and 2021
- Figure 5: Total Number of Reference Antibodies Detected between 2017 and 2021
- Figure 6: Frequency of Reference Antibodies Detected between 2017 and 2021
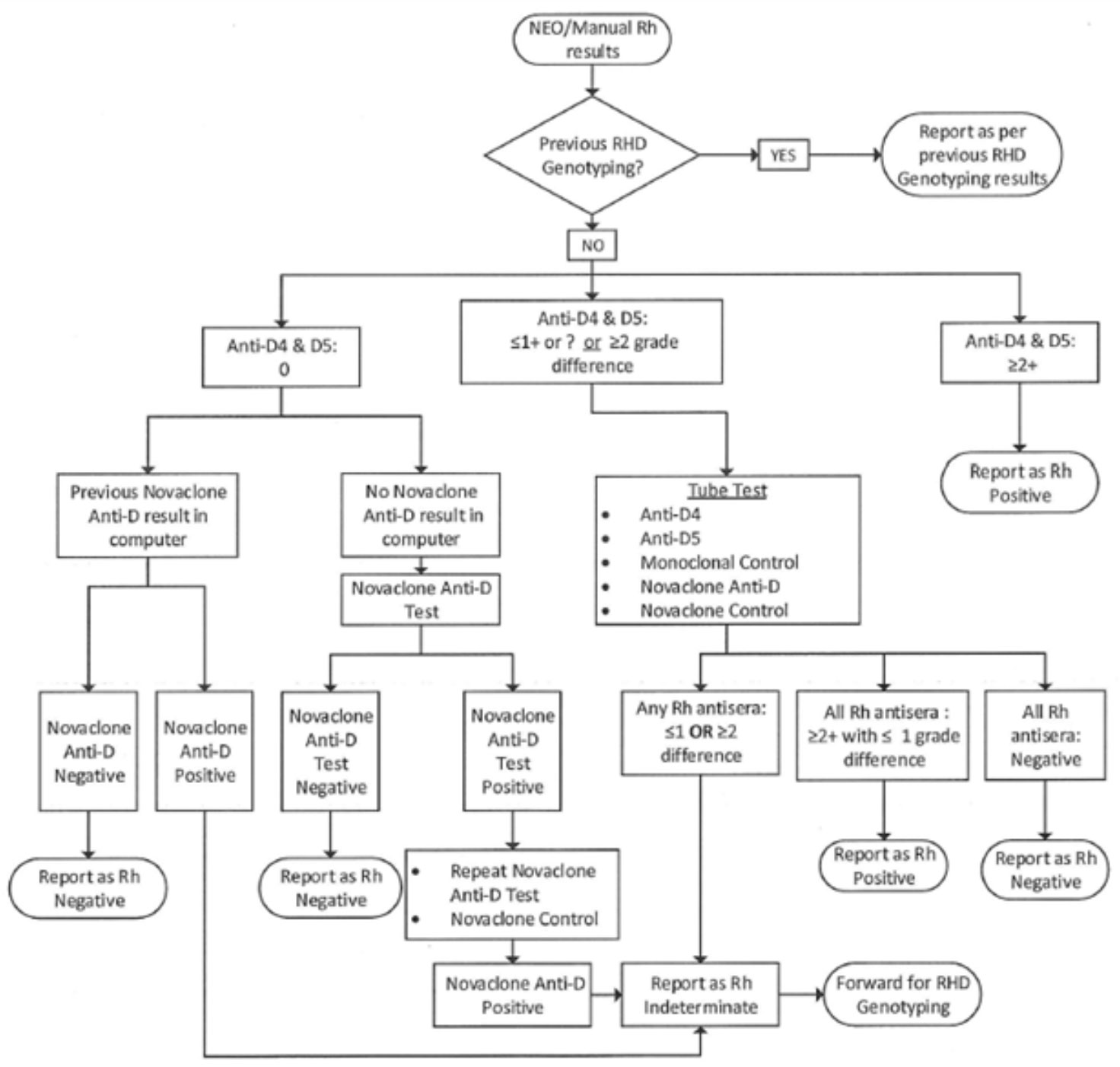
- Figure 7: RhD Testing Algorithm
- Figure 8: Turnaround Time for Perinatal Routine Samples between 2017 and 2021
- Figure 9: Turnaround Time for Reference Testing between 2017 and 2021
- Figure 10: Perinatal Rejection Reasons in Year 2021
- Figure 11: Reference Rejection Reasons in Year 2021
Tables
- Table 1: Total Number of Perinatal Specimens and Patients Tested between 2017 and 2021
- Table 2: Total Number of Clinically Significant and Insignificant Perinatal Antibodies Detected between 2017 and 2021
- Table 3: Frequency of Clinically Significant Antibodies Detected between 2017 and 2021
- Table 4: Perinatal Patient Antibody Titres Performed in Year 2021 and changed from Non-critical Level to Critical Level
- Table 5: Combination Antibodies Detected in Perinatal Patients in 2021
- Table 6: Total Reference Specimens Tested by Vancouver Diagnostic Services between 2017 and 2021
- Table 7: Total Number of Reference Antibodies Detected
- Table 8: Frequency of Reference Antibodies Detected between 2017 and 2021
- Table 9: Combination Reference Antibodies Detected in 2021
- Table 10: Fetal Genotyping Results Summary from year 2021
- Table 11: Fetal Genotyping Results Totals 2021
- Table 12: Patient # - RHD Type/Result 2021
- Table 13: RHD Genotyping – Number of Rh Negative and Rh Positive Predicted Phenotypes
- Table 14: Turnaround Time from when specimens are received at Canadian Blood Services in Vancouver to the time when the results are available – Routine Criteria by Specimen Type
- Table 15: Turnaround Time from when specimens are received at Canadian Blood Services in Vancouver to the time when the results are available – Routine Perinatal Specimens TAT between 2017 and 2021
- Table 16: Turnaround Time from when specimens are received at Canadian Blood Services in Vancouver to the time when the results are available – Reference Specimens TAT between 2017 and 2021
- Table 17: Turnaround Time for Routine Perinatal Specimens between 2017 and 2021
- Table 18: Turnaround Time for Reference Specimens between 2017 and 2021
- Table 19: Quarterly Rejection Rates – Perinatal Specimens in Year 2021
- Table 20: Quarterly Rejection Rates – Reference Specimens 2021
Perinatal Laboratory
The Perinatal Laboratory within Diagnostic Services at Canadian Blood Services provides diagnostic testing of perinatal samples for blood type and red blood cell antibodies. Results from this screening assist physicians, midwives, and nurse practitioners in ensuring the appropriate RhIG treatment recommendation and the management of pregnancy when antibodies to red cell antigens are present.
A. Testing Performed
Canadian Blood Services Perinatal Laboratory routinely performs the following tests:
- ABO/Rh blood type
- Screen for red blood cell antibodies
- Antibody Identification, if antibodies are detected
- Antibody Identification referrals
- Antibody Titration, if a clinically significant antibody is identified
- Phenotyping
Automated ABO/Rh, Antibody Screen, and Antibody Identification assays are routinely performed on the Immucor NEO Iris analyzer (hemagglutination testing and solid phase). Manual follow up testing includes the use of PEG, LISS and other methods.
B. Testing Frequency
Prenatal – Initial Testing: All patients should be tested upon their first prenatal visit.
Prenatal – 26-28 Weeks Gestation: All Rh-negative patients should be retested at 26-28 weeks gestation. Rh positive patients should also be retested at 26-28 weeks gestation when there is only one blood group result available (usually first pregnancy) or if patient is at increased risk of allo-immunization (e.g., previous transfusion, trauma, obstetrical procedure, or fetal maternal hemorrhage).
Prenatal – Antibody Present: If the antibody is known to cause HDFN, it is recommended that specimens be submitted every month followed by biweekly in the last trimester for the duration of the pregnancy dependant on the specificity of the antibody and the strength of the antibody titre.
For patients with titers of 16 or greater (and dependant on paternal phenotype) referral to Maternal Fetal Medicine clinic is recommended. Less frequent sampling may also be recommended for antibodies that are unlikely to be clinically significant or in cases where clinical monitoring through fetal Doppler ultrasound has commenced.
Refer to Fetal Genotyping (page 21) for additional information.
Postnatal: Following delivery, specimens from the patient and baby should be tested if the Rh of the patient is unknown, the patient is Rh negative, the patient has a clinically significant antibody or if the baby shows signs of HDFN (i.e., anemia or jaundice).
Partners: When a prenatal patient has an antibody capable of causing HDFN, specimens from the partner will be requested for ABO/Rh and antigen phenotyping. This will assist in assessing the probability of the baby being affected by the antibody. Partners’ specimens may also be tested to assess Rh Immune Globulin (RhIG) eligibility of Rh-negative patients.
C. Specimens Tested
The data includes all perinatal patients tested, including referrals. The data in this report reflects a calendar year period to enable better correlation to other government statistical data (Statistics Canada birth statistics).
Figure 1: Total Number of Perinatal Specimens Tested between 2017 and 2021

Table 1: Total Number of Perinatal Specimens and Patients Tested between 2017 and 2021
|
Specimen Type |
Test Type |
2017 |
2018 |
2019 |
2020 |
2021 |
|---|---|---|---|---|---|---|
|
Perinatal |
Perinatal-Type and Screen |
67,229 |
68,099 |
69,668 |
72,263 |
73, 061 |
|
Partner |
Partner-ABO/Rh |
671 |
624 |
631 |
609 |
696 |
|
Cord |
ABO/Rh |
Not reported |
Not reported |
Not reported |
4 |
3 |
|
Total # of Specimens Tested |
|
67,899 |
68,723 |
70,299 |
72,876 |
73, 760 |
|
Total # of Patients Tested |
|
62,063 |
64,992 |
69,624 |
60,677 |
59.891 |
Text Version – Table 1
Total number of perinatal specimens and patients tested between 2017 and 2021 includes specimen types Perinatal, Partner and Cord. Perinatal specimens were tested for Type and Screen. Total number of perinatal specimens tested in 2017 were 67229, in 2018 – number of perinatal specimens were 68099, in 2019 – number of perinatal specimens were 69668, in 2020 – number of perinatal specimens were 72263 and in 2021, number of perinatal specimens were 73061. Partner specimens were tested for ABO/Rh. Total number of partner specimens tested in 2017 were 671, in 2018 – number of partner specimens were 624, in 2019 – number of partner specimens were 631, in 2020 – number of partner specimens were 609 and in 2021, number of perinatal specimens were 696. Cord specimens were also tested for ABO/Rh in 2020 and 2021. Total number of cord specimens tested in 2020 were 4 and in 2021 – number of cord specimens were 3. ABO/Rh testing for Cord samples in 2017, 2018 and 2019 was not reported. Total number of patients tested 2017 were 62063, in 2018 – total number of patients tested were 64992, in 2019 - total number of patients tested were 69624, in 2020 – total number of patients tested were 60677 and in 2021, total number of patients tested were 59891.
D. Antibodies Identified
In 2021, a total of 395 antibodies were reported (see Table 2). This is less than 2020. Three hundred and fifty-seven patients (357) had antibodies identified during their pregnancies (decreased from 381 in 2020), of these; 259 patients had clinically significant antibodies, 64 had clinically insignificant antibodies and 62 patients had multiple antibodies. Passive anti-D data has been excluded from the preceding numbers. Antibodies identified were considered to be clinically significant if they have been reported to cause HDFN. The most common clinically significant antibodies identified were: anti-D, anti-E, anti-c, anti-K, (see Figure 2) which together represented 62% of the total antibodies identified. IgG Anti-M can also be considered clinically significant as it may cause HDFN and/or delayed anemia in rare cases.
Titres for 11 of the clinically significant antibodies increased from non-critical to critical levels during the pregnancy with a total of 26 antibody titres at critical levels (see Table 4). Recommendations were made for all patients with a critical titre level (current or previous pregnancy) and all Kell system antibodies to be referred to a High Risk Fetal Assessment Clinic for further follow-up and monitoring during pregnancy.
Figure 2: Total Number of Clinically Significant Perinatal Antibodies Detected between 2017 and 2021

Table 2: Total Number of Clinically Significant and Insignificant Perinatal Antibodies Detected between 2017 and 2021
|
Perinatal Antibodies Identified |
|||||
|---|---|---|---|---|---|
|
Clinically Significant Antibodies |
2017 |
2018 |
2019 |
2020 |
2021 |
|
Anti-D |
52 |
48 |
39 |
54 |
41 |
|
Anti-C |
7 |
26 |
11 |
11 |
8 |
|
Anti-Cw |
1 |
0 |
2 |
3 |
1 |
|
Anti-Ce |
0 |
0 |
0 |
|
1 |
|
Anti-c |
30 |
65 |
26 |
27 |
30 |
|
Anti-E |
101 |
150 |
80 |
72 |
60 |
|
Anti-e |
2 |
4 |
6 |
4 |
5 |
|
Anti-G |
4 |
6 |
7 |
7 |
6 |
|
Anti-K |
41 |
70 |
55 |
38 |
37 |
|
Anti-Kpa |
1 |
2 |
0 |
|
0 |
|
Anti-Lub |
0 |
2 |
0 |
|
0 |
|
Anti-M* |
49 |
52 |
37 |
38 |
35 |
|
Anti-S |
8 |
13 |
11 |
10 |
9 |
|
Anti-s |
1 |
0 |
0 |
|
1 |
|
Anti-U |
0 |
2 |
0 |
|
0 |
|
Anti-Fya |
8 |
12 |
7 |
4 |
3 |
|
Anti-Fyb |
1 |
3 |
1 |
2 |
1 |
|
Anti-Jka |
23 |
28 |
17 |
16 |
19 |
|
Anti-Jkb |
8 |
4 |
8 |
6 |
8 |
|
Anti-Jk3 |
0 |
0 |
2 |
1 |
0 |
|
Anti-Vw |
0 |
0 |
0 |
|
0 |
|
Anti-Wra |
3 |
4 |
4 |
2 |
1 |
|
Anti-Jra |
0 |
0 |
0 |
|
0 |
|
Anti-Inb |
0 |
0 |
0 |
|
0 |
|
Anti-Sc1 |
0 |
0 |
0 |
1 |
1 |
|
Anti-Lua |
1 |
2 |
0 |
1 |
0 |
|
Anti-Cob |
0 |
0 |
1 |
|
0 |
|
Anti-Dantu |
0 |
0 |
1 |
2 |
0 |
|
Anti-Joa |
0 |
1 |
0 |
|
0 |
|
Anti-Mur |
0 |
1 |
0 |
1 |
1 |
|
Anti-PP1Pk |
0 |
1 |
0 |
|
0 |
|
Anti-Yta |
1 |
2 |
0 |
|
0 |
|
Anti-Lu14 |
0 |
0 |
0 |
2 |
1 |
|
Anti-Dia |
0 |
0 |
0 |
2 |
0 |
|
Anti-Mit |
0 |
0 |
0 |
1 |
0 |
|
Total |
342 |
498 |
315 |
300 |
269 |
*Anti-M – IgG antibody component detected
|
Clinically Insignificant Antibodies |
2017 |
2018 |
2019 |
2020 |
2021 |
|---|---|---|---|---|---|
|
Anti-A1 |
11 |
9 |
9 |
15 |
12 |
|
Anti-Lea |
11 |
20 |
7 |
11 |
5 |
|
Anti-Leb |
5 |
3 |
5 |
4 |
4 |
|
Anti-N |
|
1 |
0 |
2 |
3 |
|
Anti-P1 |
19 |
2 |
6 |
6 |
10 |
|
Anti-Sda |
|
0 |
0 |
|
0 |
|
Antibody to an HLA related antigen |
Not reported |
Not reported |
Not reported |
5 |
0 |
|
Cold Agglutinin |
Not reported |
Not reported |
Not reported |
11 |
9 |
|
Not reported |
Not reported |
Not reported |
44 |
32 |
|
|
Unidentified antibody |
Not reported |
Not reported |
Not reported |
54 |
51 |
|
Passive Anti-D (not included in totals) |
726 |
588 |
687 |
719 |
594 |
|
TOTAL: Clinically Insignificant Antibodies |
46 |
35 |
27 |
152 |
126 |
Figure 3: Frequency of Clinically Significant Antibodies Detected between 2017 and 2021

Table 3: Frequency of Clinically Significant Antibodies Detected between 2017 and 2021
|
|
2017 |
2018 |
2019 |
2020 |
2021 |
|---|---|---|---|---|---|
|
Anti-D |
15.2% |
9.6% |
12.4% |
18.0% |
15.2% |
|
Anti-C |
2.0% |
5.2% |
3.5% |
3.7% |
3.0% |
|
Anti-Cw |
0.3% |
0.0% |
0.6% |
1.0% |
0.4% |
|
Anti-Ce |
0.0% |
0.0% |
0.0% |
0.0% |
0.4% |
|
Anti-c |
8.8% |
13.1% |
8.3% |
9.0% |
11.2% |
|
Anti-E |
29.5% |
30.1% |
25.4% |
24.0% |
22.3% |
|
Anti-e |
0.6% |
0.8% |
1.9% |
1.3% |
1.9% |
|
Anti-G |
1.2% |
1.2% |
2.2% |
2.3% |
2.2% |
|
Anti-K |
12.0% |
14.1% |
17.5% |
12.7% |
13.8% |
|
Anti-Kpa |
0.3% |
0.4% |
0.0% |
0.0% |
0.0% |
|
Anti-Lub |
0.0% |
0.4% |
0.0% |
0.0% |
0.0% |
|
Anti-M* |
14.3% |
10.4% |
11.7% |
12.7% |
13.0% |
|
Anti-S |
2.3% |
2.6% |
3.5% |
3.3% |
3.3% |
|
Anti-s |
0.3% |
0.0% |
0.0% |
0.0% |
0.4% |
|
Anti-U |
0.0% |
0.4% |
0.0% |
0.0% |
0.0% |
|
Anti-Fya |
2.3% |
2.4% |
2.2% |
1.3% |
1.1% |
|
Anti-Fyb |
0.3% |
0.6% |
0.3% |
0.7% |
0.4% |
|
Anti-Jka |
6.7% |
5.6% |
5.4% |
5.3% |
7.1% |
|
Anti-Jkb |
2.3% |
0.8% |
2.5% |
2.0% |
3.0% |
|
Anti-Jk3 |
0.0% |
0.0% |
0.6% |
0.3% |
0.0% |
|
Anti-Vw |
0.0% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Anti-Wra |
0.9% |
0.8% |
1.3% |
0.7% |
0.4% |
|
Anti-Jra |
0.0% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Anti-Inb |
0.0% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Anti-Sc1 |
0.0% |
0.0% |
0.0% |
0.3% |
0.4% |
|
Anti-Lua |
0.3% |
0.4% |
0.0% |
0.3% |
0.0% |
|
Anti-Cob |
0.0% |
0.0% |
0.3% |
0.0% |
0.0% |
|
Anti-Dantu |
0.0% |
0.0% |
0.3% |
0.7% |
0.0% |
|
Anti-Joa |
0.0% |
0.2% |
0.0% |
0.0% |
0.0% |
|
Anti-Mur |
0.0% |
0.2% |
0.0% |
0.3% |
0.4% |
|
Anti-PP1Pk |
0.0% |
0.2% |
0.0% |
0.0% |
0.0% |
|
0.3% |
0.4% |
0.0% |
0.0% |
0.0% |
|
|
Anti-Lu14 |
0.0% |
0.0% |
0.0% |
0.7% |
0.4% |
|
Anti-Dia |
0.0% |
0.0% |
0.0% |
0.7% |
0.0% |
|
Anti-Mit |
0.0% |
0.0% |
0.0% |
0.3% |
0.0% |
Table 4: Perinatal Patient Antibody Titres Performed in Year 2021 and changed from Non-critical Level to Critical Level
|
Critical Level |
Non-Critical Level |
Non-Critical to Critical |
|
|---|---|---|---|
|
Anti-C |
2 |
21 |
2 |
|
Anti-c |
|
3 |
|
|
Anti-Ce |
|
2 |
|
|
Anti-cE |
|
1 |
|
|
Anti-CG |
|
|
|
|
Anti-Cw |
|
1 |
|
|
Anti-D |
6 |
44 |
4 |
|
Anti-DC |
3 |
1 |
|
|
Anti-DG |
5 |
|
1 |
|
Anti-DG |
|
|
|
|
Anti-Dia |
|
|
|
|
Anti-E |
6 |
48 |
3 |
|
Anti-e |
|
5 |
|
|
Anti-Ec |
3 |
5 |
|
|
Anti-Fya |
|
1 |
|
|
Anti-Fyb |
|
1 |
|
|
Anti-G |
|
1 |
1 |
|
Anti-Jk3 |
|
|
|
|
Anti-Jka |
|
18 |
|
|
Anti-Jkb |
|
9 |
|
|
Anti-Lu14 |
|
1 |
|
|
Anti-Lua |
|
|
|
|
Anti-M |
|
33 |
|
|
Anti-Mit |
|
|
|
|
Anti-Mur |
|
|
|
|
Anti-S |
|
8 |
|
|
|
1 |
|
|
|
Anti-Sc1 |
|
1 |
|
|
Anti-Wra |
1 |
|
|
|
Totals |
26 |
205 |
11 |
Table 5: Combination Antibodies Detected in Perinatal Patients in 2021
|
Combination Antibodies |
Prenatal |
|---|---|
|
Anti-C, Unidentified Antibody |
1 |
|
Anti-Anti-P1, Anti-K, Unidentified Antibody |
1 |
|
Anti-C, Anti-e |
1 |
|
Anti-c, Anti-Jka, Warm Autoantibody |
1 |
|
Anti-C, Wra, Unidentified Antibody |
1 |
|
Anti-D, Anti-C |
1 |
|
Anti-D, Anti-C, Anti-Jkb |
1 |
|
Anti-D, Anti-C, Unidentified Antibody |
1 |
|
Anti-D, Anti-G |
2 |
|
Anti-D, Anti-G, Unidentified Antibody |
4 |
|
Anti-D, Anti-P1 |
2 |
|
Anti-D, Unidentified Antibody |
1 |
|
Anti-E, Anti-c |
8 |
|
Anti-E, Anti-c, Anti-K, Anti-Jka |
1 |
|
Anti-e, Anti-Ce |
1 |
|
Anti-E, Anti-Jka |
1 |
|
Anti-E, Anti-Lea, Anti-K |
1 |
|
Anti-e, Anti-P1 |
1 |
|
Anti-E, Anti-S |
1 |
|
Anti-E, Unidentified Antibody |
1 |
|
Anti-Fyb, Anti-Jka, Unidentified Antibody |
1 |
|
Anti-Jka, Unidentified Antibody |
3 |
|
Anti-Jkb, Unidentified Antibody |
1 |
|
Anti-K, Unidentified Antibody |
1 |
|
Anti-Lea, Anti-Jka |
1 |
|
Anti-Lea, Anti-Leb |
1 |
|
Anti-Lea, Anti-Leb, Unidentified Antibody |
1 |
|
Anti-M, Anti-Fya |
1 |
|
Anti-M, Anti-K |
1 |
|
Anti-M, Unidentified Antibody |
3 |
|
Anti-s, Anti-Jka, Unidentified Antibody |
1 |
|
3 |
|
|
Cold Agglutinin, Unidentified Antibody |
1 |
|
Warm Autoantibody, Cold Agglutinin |
1 |
|
Warm Autoantibody, Unidentified Antibody |
1 |
Reference Laboratory
The Reference Laboratory, Vancouver Diagnostic Services provides testing for hospital transfusion medicine laboratories. Hospital patients who are repeatedly transfused may develop red cell antibodies and as a result may have difficulty in tolerating transfusions. Diagnostic Services has specialized and experienced technologists that assist and provide consultation to hospital transfusion medicine laboratories (24 hours, 7 days per week). The Reference Laboratory identifies red cell antibodies and provides transfusion recommendations. Diagnostic Services has a varied selection of specialized procedures and rare reagents to resolve more difficult red cell antibody cases. Staff within our department may collaborate with other references laboratories such as the National Immunohematology Reference laboratory (NIRL).
Diagnostic Services Red Cell Antibody Investigations
In 2021, hospitals have referred 401 requests for red cell antibody identification.
Diagnostic Services provides support for all BC and Yukon hospitals. Referring hospitals have different capabilities and expertise in resolving red cell antibody investigations. Some hospitals have limited reagents for antibody identification or phenotyping of patient or donor units. Others have access to a wider variety of reagent red cell panels and methods as well as on site immunohematology expertise. A few hospital transfusion medicine laboratories have the resources to resolve the majority of serological problems and send only complex investigations for additional serological or genotyping studies.
Canadian Blood Services, Diagnostic Services provides consultation and testing support including antibody investigation, advanced or alternative techniques where required, and recommendations for compatibility testing methods and selection of appropriate donor unit phenotypes if necessary.
Reporting may include interim, final and supplemental reports, depending on the urgency of the testing, the need for patient transfusion and the complexity of the investigation. When a new antibody is identified by the Diagnostic Services Laboratory, a patient wallet card may be provided.
A. The Testing Performed to support patient referral investigations includes:
- ABO/Rh blood type and discrepancy investigations (if required)
- Screen for red blood cell antibodies
- Antibody Identification
- Phenotyping (patient and donor units)
- Transfusion Reaction Investigation
- Direct Antiglobulin Test
- Elution
- Allo and Auto Adsorptions
- Neutralization Tests
- Referral Genotype Testing
Antibody Screening is routinely performed by solid phase testing. A combination of solid phase testing and indirect antiglobulin tube testing using PEG for enhancement are the primary antibody identification methods. Gel IAT testing may also be used.
Figure 4 : Total Reference Specimens Tested by Vancouver Diagnostic Services between 2017 and 2021

Table 6: Total Reference Specimens Tested by Vancouver Diagnostic Services between 2017 and 2021
|
Specimen Type |
2017 |
2018 |
2019 |
2020 |
2021 |
|---|---|---|---|---|---|
|
Total Reference Antibody Investigations |
412 |
315 |
437 |
428 |
401 |
B. Antibodies Identified
In 2021, a total of 436 antibodies were reported (see Table 7). The total number of antibodies detected is the same as 2020, and the distribution of the most common antibodies remains consistent. Four hundred and seventeen (417) patients had antibodies identified; of these, two hundred and seventy-two (272) patients had multiple antibodies. Antibodies identified were considered to be clinically significant if they have been reported to cause acute or delayed hemolytic transfusion reactions. The most common clinically significant antibodies identified were: anti-D, anti-E, anti-K, anti-c, anti-Fya (see Figure 5) which together represented 22% of the total antibodies identified.
Investigation of warm autoantibodies is a frequent request. Techniques including such as auto and alloadsorption may be used along with DTT treatment of screening or panel cells for anti CD38-related panreactivity.
Figure 5: Total Number of Reference Antibodies Detected between 2017 and 2021

Table 7: Total Number of Reference Antibodies Detected
Figure 6: Frequency of Reference Antibodies Detected between 2017 and 2021

Table 8: Frequency of Reference Antibodies Detected between 2017 and 2021
|
Antibodies |
2017 |
2018 |
2019 |
2020 |
2021 |
|---|---|---|---|---|---|
|
Anti-D |
12.7% |
5.8% |
21.0% |
2.5% |
1.4% |
|
Anti-A1 |
2.7% |
3.5% |
0.8% |
0.0% |
0.5% |
|
Anti-C |
1.7% |
8.1% |
4.2% |
4.4% |
2.8% |
|
Anti-c |
7.4% |
7.7% |
5.5% |
2.8% |
3.0% |
|
Anti-Ce |
0.0% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Anti-Ch |
0.0% |
0.0% |
0.0% |
0.2% |
0.5% |
|
Anti-Cob |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Anti-Cw |
0.2% |
1.2% |
0.8% |
1.6% |
0.5% |
|
Anti-Dantu |
0.0% |
0.0% |
0.4% |
0.0% |
0.0% |
|
Anti-Dia |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Anti-E |
24.8% |
15.4% |
17.6% |
9.2% |
9.2% |
|
Anti-e |
0.5% |
2.3% |
2.9% |
0.5% |
2.1% |
|
Anti-f |
0.0% |
0.0% |
0.4% |
0.0% |
0.0% |
|
Anti-Fya |
2.0% |
5.8% |
5.0% |
1.8% |
2.3% |
|
Anti-Fyb |
0.2% |
0.8% |
1.3% |
0.7% |
1.4% |
|
Anti-Fy3 |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Anti-G |
1.0% |
4.2% |
2.9% |
1.6% |
1.4% |
|
Anti-Ina |
0.0% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Anti-Inb |
0.0% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Anti-Jk3 |
0.0% |
1.2% |
0.4% |
0.2% |
0.0% |
|
Anti-Jka |
5.6% |
3.8% |
4.2% |
3.2% |
2.5% |
|
Anti-Jkb |
2.0% |
2.3% |
1.3% |
0.5% |
1.4% |
|
Anti-JMH |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Anti-Jra |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Anti-K |
10.0% |
10.0% |
9.7% |
6.0% |
5.3% |
|
Anti-k |
0.0% |
0.4% |
0.0% |
0.2% |
0.0% |
|
Anti-Kpa |
0.2% |
0.4% |
0.4% |
1.1% |
0.7% |
|
Anti-Kpb |
0.0% |
0.4% |
0.0% |
0.0% |
0.0% |
|
Anti-Lea |
2.7% |
7.7% |
0.8% |
0.7% |
0.7% |
|
Anti-Leb |
1.2% |
1.2% |
0.4% |
0.5% |
0.2% |
|
Anti-Lua |
0.2% |
0.0% |
0.8% |
0.2% |
1.1% |
|
Anti-Lub |
0.0% |
0.0% |
0.8% |
0.0% |
0.0% |
|
Anti-Lu14 |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Anti-LW |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Anti-M |
12.0% |
3.8% |
2.5% |
2.5% |
1.4% |
|
Anti-McCd/ Anti-Vil |
0.0% |
0.0% |
0.4% |
0.5% |
0.0% |
|
Anti-Mia |
0.0% |
0.8% |
0.0% |
0.0% |
0.5% |
|
Anti-Mur |
0.0% |
0.4% |
0.0% |
0.0% |
0.2% |
|
Anti-N |
0.0% |
0.4% |
0.4% |
0.2% |
0.0% |
|
Anti-P1 |
4.7% |
0.8% |
0.8% |
1.1% |
0.2% |
|
Anti-S |
2.0% |
3.5% |
2.5% |
1.8% |
3.7% |
|
Anti-s |
0.2% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Anti-Sc1 |
0.0% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Anti-Sda |
0.0% |
0.0% |
0.8% |
0.0% |
0.0% |
|
Anti-U |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Anti-V |
0.2% |
0.0% |
0.0% |
0.0% |
0.2% |
|
Anti-Vel |
0.0% |
0.0% |
0.0% |
0.2% |
0.2% |
|
Anti-Vw |
0.0% |
0.4% |
0.0% |
0.0% |
0.0% |
|
Anti-Wra |
0.7% |
0.8% |
1.3% |
0.9% |
1.4% |
|
Anti-Yta |
0.2% |
0.0% |
0.0% |
0.0% |
0.0% |
|
Antibody to a Low Prevalence Antigen |
0.0% |
0.0% |
0.0% |
0.2% |
0.0% |
|
Antibody to an HLA related antigen |
0.0% |
0.0% |
0.0% |
0.2% |
0.5% |
|
Autoantibody |
0.0% |
0.0% |
0.0% |
0.2% |
0.2% |
|
0.0% |
0.0% |
0.0% |
30.0% |
31.4% |
|
|
Cold Agglutinin |
0.0% |
0.0% |
0.0% |
7.6% |
8.3% |
|
Unidentified antibody |
0.0% |
0.0% |
0.0% |
8.5% |
10.1% |
|
Passive Anti-D |
4.7% |
7.3% |
9.2% |
6.2% |
4.4% |
Table 9: Combination Reference Antibodies Detected in 2021
|
Combination Antibodies |
Serology |
|---|---|
|
Antibody to an HLA related antigen, Unidentified Antibody |
1 |
|
Anti-C, Anti-D, Anti-Fya |
1 |
|
Anti-C, Anti-D, Warm Autoantibody |
1 |
|
Anti-C, Anti-E, Anti-Jka |
1 |
|
Anti-C, Anti-E, Anti-K |
2 |
|
Anti-C, Anti-e, Unidentified Antibody |
1 |
|
Anti-c, Anti-Fya, Cold Agglutinin |
1 |
|
Anti-C, Anti-G |
3 |
|
Anti-C, Anti-K, Anti-S, Anti-Lea, Warm Autoantibody |
1 |
|
Anti-C, Unidentified Antibody |
1 |
|
Anti-C, Warm Autoantibody |
2 |
|
Anti-Ch, Anti-Fya |
1 |
|
Anti-Cw, Anti-E, Anti-K, Anti-S, Anti-Jkb, Warm Autoantibody |
1 |
|
Anti-D, Anti-G |
2 |
|
Anti-E, Anti-c |
2 |
|
Anti-E, Anti-c, Anti-Cw, Anti-S, Unidentified Antibody |
1 |
|
Anti-E, Anti-c, Anti-Fya |
1 |
|
Anti-E, Anti-c, Anti-Jka, Warm Autoantibody |
1 |
|
Anti-E, Anti-c, Anti-Jkb, Warm Autoantibody, Cold Agglutinin |
1 |
|
Anti-E, Anti-c, Anti-K, Warm Autoantibody |
1 |
|
Anti-E, Anti-c, Anti-K, Warm Autoantibody, Unidentified Antibody |
1 |
|
Anti-E, Anti-c, Anti-M, Warm Autoantibody |
1 |
|
Anti-E, Anti-c, Anti-S, Anti-Jka, Warm Autoantibody |
1 |
|
Anti-E, Anti-Fya, Warm Autoantibody |
2 |
|
Anti-e, Anti-Jka, Warm Autoantibody, Unidentified Antibody |
1 |
|
Anti-E, Anti-Jkb, Unidentified Antibody |
1 |
|
Anti-E, Anti-K, Anti-Jka, Anti-Lua |
1 |
|
Anti-E, Anti-K, Anti-Jka, Warm Autoantibody |
1 |
|
Anti-E, Anti-K, Anti-Jka, Warm Autoantibody, Unidentified Antibody |
1 |
|
Anti-E, Anti-K, Anti-Lua |
1 |
|
Anti-e, Anti-K, Anti-M |
1 |
|
Anti-E, Anti-K, Cold Agglutinin |
1 |
|
Anti-E, Anti-K, Warm Autoantibody |
1 |
|
Anti-e, Anti-P1 |
1 |
|
Anti-E, Anti-S, Anti-Kpa |
1 |
|
Anti-E, Anti-S, Unidentified Antibody |
1 |
|
Anti-E, Anti-Wra, Warm Autoantibody |
1 |
|
Anti-e, Cold Agglutinin |
1 |
|
Anti-E, Unidentified Antibody |
1 |
|
Anti-E, Warm Autoantibody |
8 |
|
Anti-e, Warm Autoantibody |
2 |
|
Anti-Fya, Warm Autoantibody |
1 |
|
Anti-Fya, Warm Autoantibody |
1 |
|
Anti-Fyb, Anti-Jka, Unidentified Antibody |
1 |
|
Anti-Fyb, Warm Autoantibody |
1 |
|
Anti-Ge2, Unidentified Antibody |
1 |
|
Anti-hrS, Anti-Jkb, Warm Autoantibody |
1 |
|
Anti-Jka, Unidentified Antibody |
1 |
|
Anti-Jkb, Warm Autoantibody |
1 |
|
Anti-K, Anti-S, Anti-Fya, Anti-Jkb, Warm Autoantibody |
1 |
|
Anti-K, Anti-S, Warm Autoantibody, Antibody to an HLA related antigen |
1 |
|
Anti-K, Anti-V |
1 |
|
Anti-K, Unidentified Antibody |
2 |
|
Anti-Kpa, Warm Autoantibody |
2 |
|
Anti-Lea, Anti-Leb |
1 |
|
Anti-Lea, Cold Agglutinin |
1 |
|
Anti-Lua, Anti-Wra, Unidentified Antibody |
1 |
|
Anti-M, Anti-S |
1 |
|
Anti-M, Warm Autoantibody |
1 |
|
Anti-S, Anti-Fyb, Anti-Lua |
1 |
|
Anti-S, Anti-Fyb, Warm Autoantibody |
1 |
|
Anti-S, Anti-Jka |
1 |
|
Anti-S, Anti-Jka, Warm Autoantibody, Cold Agglutinin |
1 |
|
Anti-S, Unidentified Antibody |
1 |
|
Anti-S, Warm Autoantibody, Cold Agglutinin, Unidentified Antibody |
1 |
|
Anti-Wra, Unidentified Antibody |
1 |
|
1 |
|
|
Cold Agglutinin, Unidentified Antibody |
1 |
|
Warm Autoantibody, Cold Agglutinin |
11 |
|
Warm Autoantibody, Unidentified Antibody |
5 |
Fetal Genotyping
Canadian Blood Services in BC refers specimens for fetal blood group genotyping on prenatal plasma to the International Blood Group Reference Laboratory (IBGRL) of the National Health Services (NHS) in Bristol, United Kingdom.
Specimens are submitted through the Maternal Fetal Medicine clinics in BC and are accepted if they meet the following criteria:
- The patient has an antibody capable of causing hemolytic disease of the fetus/newborn (HDFN), AND
- The partner is heterozygous for the corresponding antigen (or unknown), AND
- The antibody titre has reached a critical level, OR
- There has been a previous fetus/newborn affected by HDFN, and
- The antibody is RH and/or anti-K
Discussion with a Canadian Blood Services physician is required prior to submitting specimens for testing outside of these criteria.
Table 10: Fetal Genotyping Results Summary from year 2021
|
Patient |
Perinatal Antibody |
Predicted Fetal Phenotype |
Follow-up Required |
|---|---|---|---|
|
1 |
Anti-D, Anti-G |
D+ |
Yes |
|
2 |
Anti-K |
K+ |
Yes |
|
3 |
Anti-D |
D+ |
Yes |
|
4 |
Anti-K |
K- |
No |
|
5 |
Anti-D |
D+ |
Yes |
|
6 |
Anti-K |
K+ |
Yes |
|
7 |
Anti-K |
N/A |
Not required. Pt. had IUT |
|
8 |
Anti-E |
E+ |
Yes |
|
9 |
Anti-D |
D+ |
Yes |
|
10 |
Anti-D, C |
D-C- |
No |
|
11 |
Anti-E, Anti-c |
E-c- |
No |
|
12 |
Anti-E |
E+ |
Yes |
|
13 |
Anti-E |
E+ |
Yes |
|
14 |
ant-D, Anti-P1 |
D- |
No |
|
15 |
Anti-D, Ant-C |
D+ |
Yes |
|
16 |
Anti-K |
K+ |
Yes |
|
Anti-E |
E+ |
Yes |
|
|
18 |
Anti-K |
N/A |
Sample thawed in transit. Repeat sample not collected, too close to delivery. |
|
19 |
Anti-D |
D+ |
Yes |
|
20 |
Anti-E, Anti-c |
E- c- |
No |
Table 11: Fetal Genotyping Results Totals 2021
|
Year |
2021 |
|---|---|
|
Total samples sent |
25 |
|
# of patients tested |
20 |
|
# of patients not requiring MFM follow-up. (Fetus tested negative for the corresponding antigen) |
5 |
RHD Red Cell Genotyping
Based on the following testing algorithm patients with a serologically variable Rh D typing results may have a genetic testing for the RHD gene. For 2021, the following results were obtained in patients using one of the two Red Cell antigen genotyping platforms available at CBS:
Text Version – Figure 7
Figure 7 describes RhD testing algorithm. If NEO/Manual Rh results and previous RHD Genotyping results are available, report RhD as per previous RHD Genotyping results.
If NEO/Manual Rh results are available but previous RHD Genotyping results are not available and Anti-D4 & Anti-D5 results are negative, check for the previous Novaclone Anti-D result in computer. If previous Novaclone Anti-D is Negative, report RhD as Rh Negative. If previous Novaclone Anti-D is positive, report as Rh Indeterminate and forward the sample for RHD Genotyping.
If NEO/Manual Rh results are available but previous RHD Genotyping results are not available and Anti-D4 & Anti-D5 results are negative, check for the previous Novaclone Anti-D result in computer. If no Novaclone Anti-D result is available in computer, perform Novaclone Anti-D Test. If Novaclone Anti-D is Negative, report RhD as Rh Negative. If Novaclone Anti-D tests positive, repeat Novaclone Anti-D Test with Novaclone Control. If repeat Novaclone Anti-D is positive, report as Rh Indeterminate and forward the sample for RHD Genotyping.
If NEO/Manual Rh results are available but previous RHD Genotyping results are not available and Anti-D4 & Anti-D5 results are less than or equal to one or equivocal or greater than or equal to two grade difference, perform tube tests for Anti-D4, Anti-D5, Monoclonal Control, Novaclone Anti-D and Novaclone Control. If any Rh Antisera results are less than or equal to one grade difference or greater than or equal to two grade difference, report as Rh Indeterminate and forward the sample for RHD Genotyping. If all the Rh antisera results are greater than or equal to two with less than or equal to one grade difference, report RhD as Rh Positive. If all antisera results are negative, report RhD as Rh Negative.
If NEO/Manual Rh results are available but previous RHD Genotyping results are not available and Anti-D4 & Anti-D5 results are greater than or equal to two, report RhD as Rh Positive.
Table 12: Patient # - RHD Type/Result 2021
|
# of Patients |
RHD Genotype |
Predicted Phenotype |
RHD Sequencing |
Rh(D) Group |
|---|---|---|---|---|
|
6 |
DAR |
D variant |
NO |
NEG |
|
1 |
DAU2 |
D Variant |
NO |
NEG |
|
1 |
DAU4 or DV type 5 |
D Variant |
NO |
NEG |
|
1 |
DAU6 |
D variant |
NO |
NEG |
|
1 |
DFR or DFR3 |
Partial D |
NO |
NEG |
|
1 |
DHMi |
D Variant |
NO |
Neg |
|
1 |
DOL or DOL2 |
D Variant |
NO |
NEG |
|
1 |
DVI |
D Variant |
NO |
NEG |
|
15 |
Possible D |
D Positive |
NO |
POS |
|
30 |
Weak D type 1 |
Weak D |
NO |
POS |
|
19 |
Weak D type 2 |
Weak D |
NO |
POS |
|
11 |
Weak D type 3 |
Weak D |
NO |
POS |
|
13 |
Weak D type 4.0 or 4.3 |
Weak D |
NO |
Neg |
|
1 |
Weak D type 4.1 |
Weak D |
NO |
NEG |
|
1 |
RHD Deletion and a Weak D Type 96 |
Weak D |
YES |
NEG |
|
3 |
Normal D |
D Positive |
NO |
POS |
|
106 |
Total number tested |
|||
The array used for RHD genotyping (Immucor’s BioArray BeadChip™ Molecular Assay) is extensive and can detect the most common mutations of the RHD gene. The most common variants detected are weak D type 1, weak D type 2 and weak D type 3. Individuals with these phenotypes can be safely treated as Rh positive as it has been established that they will not form alloanti-D. Patients with any other weak or partial D phenotypes may be capable of forming alloanti-D and should be treated as Rh negative. When none of the variants present on the array are detected, the software will produce a result of “Possible D”. When none of the variants present on the array are detected, the software will produce a result of “Possible D”. Prior to 2018, Canadian Blood Services recommended that patients with a result of “Possible D” be treated as Rh negative. However, based on clinical experience at that time, the reporting was changed in 2018 such that patients with a result of “Possible D” were reported as Rh Positive. Categorization of “Possible D” individuals is under continuing review as more experience is gained with the assay, and sequencing to resolve difficult cases becomes more readily available.
Table 13: RHD Genotyping – Number of Rh Negative and Rh Positive Predicted Phenotypes
|
|
2019 |
2020 |
2021 |
|---|---|---|---|
|
Rh Positive |
106 |
114 |
78 |
|
Rh Negative |
24 |
30 |
28 |
|
Total # samples tested |
130 |
144 |
106 |
Note: Data not captured prior to 2019
A. Turnaround Times
To ensure timely reporting of patient test results, Canadian Blood Services monitors turnaround time (TAT) from when the specimen is received at Canadian Blood Services in Vancouver to the time when the results are available. Since monitoring of this quality indicator began in 2008, the percentage of specimens has consistently exceeded the predefined TAT threshold. Samples whose testing exceeds the expected TAT are usually those where clinically significant antibodies are detected or where difficulty in finding compatible blood is encountered.
Table 14: Turnaround Time from when specimens are received at Canadian Blood Services in Vancouver to the time when the results are available – Routine Criteria by Specimen Type
|
Specimen Type |
Expected Turnaround Time |
Expected % of Specimens Which Meet or Exceed Expected TAT |
|---|---|---|
|
Routine Perinatal |
< 72 hours |
85% |
|
Reference Testing |
<72 hours |
85% |
Table 15: Turnaround Time from when specimens are received at Canadian Blood Services in Vancouver to the time when the results are available – Routine Perinatal Specimens TAT between 2017 and 2021
|
Turnaround Time (TAT) |
2017 |
2018 |
2019 |
2020 |
2021 |
|---|---|---|---|---|---|
|
% of Specimens Tested within 72 hours |
90% |
89% |
88% |
89% |
89% |
|
% of Specimens Tested > 72 hours |
10% |
11% |
12% |
11% |
11% |
Table 16: Turnaround Time from when specimens are received at Canadian Blood Services in Vancouver to the time when the results are available – Reference Specimens TAT between 2017 and 2021
|
Turn Around Time (TAT) |
2017 |
2018 |
2019 |
2020 |
2021 |
|---|---|---|---|---|---|
|
% of Specimens Tested within 72 hours |
98% |
99% |
100% |
100% |
99% |
|
% of Specimens Tested > 72 hours |
2% |
1% |
0% |
0% |
1% |
Figure 8: Turnaround Time for Routine Perinatal Specimens between 2017 and 2021

Table 17: Turnaround Time for Routine Perinatal Specimens between 2017 and 2021
|
Year |
Q1 (Jan-Mar) |
Q2 (Apr - Jun) |
Q3 (Jul - Sept) |
Q4 (Oct -Dec) |
%<72 hours |
%>72 hours |
|---|---|---|---|---|---|---|
|
2017 |
91% |
90% |
88% |
91% |
90% |
10% |
|
91% |
89% |
89% |
88% |
89% |
11% |
|
|
2019 |
87% |
87% |
87% |
91% |
88% |
12% |
|
2020 |
87% |
92% |
88% |
87% |
89% |
12% |
|
2021 |
90% |
88% |
90% |
88% |
89% |
11% |
Figure 9: Turnaround Time for Reference Specimens between 2017 and 2021

Table 18: Turnaround Time for Reference Specimens between 2017 and 2021
|
Year |
Q1 (Jan-Mar) |
Q2 (Apr - Jun) |
Q3 (Jul - Sept) |
Q4 (Oct -Dec) |
%<72 hours |
%>72 hours |
|---|---|---|---|---|---|---|
|
2017 |
99% |
98% |
97% |
99% |
98% |
2% |
|
99% |
99% |
99% |
99% |
99% |
1% |
|
|
2019 |
100% |
100% |
99% |
100% |
100% |
0% |
|
2020 |
100% |
99% |
100% |
100% |
100% |
0% |
|
2021 |
99% |
100% |
99% |
100% |
100% |
1% |
B. Rejected Specimens
Each time a specimen is rejected, a reason for rejection is entered into our Laboratory Information System. This data is then retrieved and analyzed on a quarterly basis. The number of rejected specimens is quite low for both perinatal and reference specimens. Reference specimens come from hospitals and perinatal samples are primarily collected at external collection sites.
For perinatal specimens, the most common reason for rejecting a sample is that the sample is a duplicate. Samples are rejected if another sample from the patient was tested within the previous week. Often a duplicate sample is collected when the patient has seen their family physician and then sees their obstetrician shortly after. We do ensure that the report from the initial testing is sent to the second physician making the request. Health care professionals can access Canadian Blood Services reports for BC patients on Care Connect (BC’s Electronic Health Record).
Figure 10: Perinatal Rejection Reasons in Year 2021

Table 19: Quarterly Rejection Rates – Perinatal Specimens in Year 2021
|
Rejection Category |
Q1 (Jan-Mar) |
Q2 (Apr - Jun) |
Q3 (Jul - Sept) |
Q4 (Oct -Dec) |
|---|---|---|---|---|
|
Requisition |
22 |
16 |
1 |
21 |
|
Specimen |
148 |
104 |
71 |
93 |
|
Discrepancies Between Requisition & Specimen |
16 |
0 |
2 |
1 |
|
Discrepancies Between Current Requisition & Historical Records |
0 |
0 |
0 |
0 |
|
2 |
3 |
8 |
5 |
|
|
Total # specimens rejected |
188 |
123 |
82 |
120 |
|
Total # specimens received |
20242 |
18298 |
17191 |
18565 |
|
Rejections as a % of total |
0.9% |
0.7% |
0.5% |
0.6% |
Figure 11: Reference Rejection Reasons in Year 2021

Table 20: Quarterly Rejection Rates – Reference Specimens 2021
|
Rejection Category |
Q1 (Jan-Mar) |
Q2 (Apr - Jun) |
Q3 (Jul - Sept) |
Q4 (Oct -Dec) |
|---|---|---|---|---|
|
Requisition |
0 |
0 |
0 |
1 |
|
Specimen |
3 |
2 |
0 |
4 |
|
Discrepancies Between Requisition & Specimen |
0 |
0 |
0 |
0 |
|
Discrepancies Between Current Requisition & Historical Records |
0 |
0 |
0 |
0 |
|
0 |
0 |
1 |
0 |
|
|
Total # specimens rejected |
3 |
2 |
1 |
5 |
|
Total # specimens received |
163 |
145 |
90 |
125 |
|
Rejections as a % of total |
1.8% |
1.4% |
1.1% |
4.0% |
Diagnostic Services Update 2021
Updates pertain to all Diagnostic Services sites within Canadian Blood Services: Vancouver, Edmonton, Winnipeg and Brampton
Presentations / Abstracts / Publications Listing
|
Lhevinne Ciurcovich, Lynnette Beaudin, Arianne Fuellos, Balkar Gill, Ilona Resz, Debra Lane, Judith Hannon, Gwen Clarke, Melanie Bodnar. Comparison of Manual SIAT vs Automated Solid Phase Methodology for Perinatal Antibody Titration. Poster, CSTM 2021 |
|
|
Lhevinne Ciurcovich1, Sarah Manfredi2, Sarah Buchko2, Darlene Mueller2, Michelle Wong2, Mohammad Bahmanyar2, MatthewYan1, Gwen Clarke1. Anti-Ina Implicated in Hemolytic Disease of the Fetus and Newborn in an Indigenous Woman. Poster, CSTM 2021
|
|
|
Lhevinne Ciurcovich, Gwen Clarke, Matthew Yan. A Case of ABO Chimerism in a Perinatal Patient. Poster, CSTM 2021 |
|
|
Lhevinne Ciurcovich. Cell-Free Fetal DNA Testing: Advantages, Challenges and Limitations. Presentation: Virtual Conference, 22nd Annual Education Day on Blood Transfusion Issues, 2021-09-24. |
|
|
Lhevinne Ciurcovich. Immunohematology Case Studies. Presentation: Immucor ImmuTECH Education Day (Virtual) 2021-05-05. |
|
|
Lynnette Beaudin, Dr. Lani Lieberman MD, FRCP, Fetal and neonatal alloimmune thrombocytopenia (FNAIT): Diagnosis, Investigation and Treatment. Presentation: U of T Monthly Transfusion Rounds (Virtual) 2021-02-25 |
|
|
Bodnar M, Hannaford K, Montemayor-Garcia C, Hannon J. Blindspots in Immucor BioArray RHD Molecular BeadChip Test: A Review of Cases at Canadian Blood Services Referred Out for RHD Gene Sequencing. Poster/Abstract, CSTM 2021 |
|
|
Floch A, Vege S, Berardi P, Hannon J, Ochoa-Garay G, Lomas-Francis C, et al. A change in RHD is associated with aberrant transcription and very weak D phenotype. Transfusion 2021 |
|
|
Flegel WA, Bodnar M, Clarke G, Hannon J, Lieberman L., ‘What constitutes the most cautious approach for a pregnant person with weak D type 4.0?’ Letter to the Editor, CMAJ June 2021 |